Global Healthcare Fraud Detection Market Size, Share, and COVID-19 Impact Analysis, By Type (Descriptive Analytics, Predictive Analytics, and Prescriptive Analytics), By Delivery Model (On-premises, Cloud-based, and Others), By Application (Insurance Claims Review, Pharmacy Billing Issues, Payment Integrity, and Others), By End User (Private Insurance Payers, Public and Government Agencies, Third Party Service Providers, and Others), and By Region (North America, Europe, Asia-Pacific, Latin America, Middle East, and Africa), Analysis and Forecast 2023 - 2033
Industry: HealthcareGlobal Healthcare Fraud Detection Market Insights Forecasts to 2033
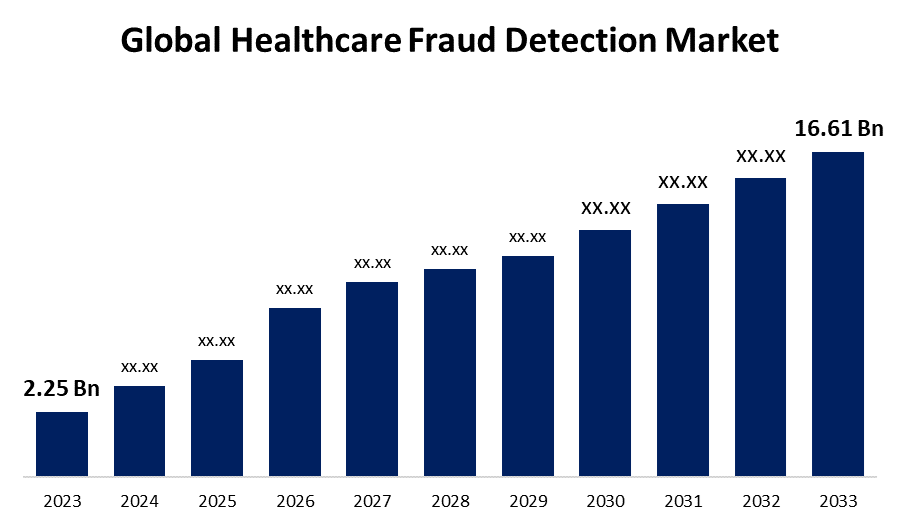
- The Global Healthcare Fraud Detection Market Size was Valued at USD 2.25 Billion in 2023
- The Market Size is Growing at a CAGR of 22.13% from 2023 to 2033
- The Worldwide Healthcare Fraud Detection Market Size is Expected to Reach USD 16.61 Billion by 2033
- Europe is Expected to Grow the fastest during the forecast period.
Get more details on this report -
The Global Healthcare Fraud Detection Market Size is Anticipated to Exceed USD 16.61 Billion by 2033, Growing at a CAGR of 22.13% from 2023 to 2033.
Market Overview
Healthcare fraud detection minimizes unnecessary payments by helping to identify and stop healthcare fraud, waste, and abuse at every step of the claim process. It integrates with current payment integrity solutions and gathers information from both internal and external sources, including watch lists, unstructured texts, third parties, and claims systems, to enable effective data management. It depends on several cutting-edge analytical and artificial intelligence (AI) methods, such as recent statistics, deep learning, machine learning (ML), and text analytics algorithms. In addition, it saves all related case data and utilizes a flexible procedure to support operational, clinical, and investigative reviews. Healthcare fraud detection, which includes account auditing and investigative work, is a collection of procedures used to prevent someone from gaining patient information or property on a fraudulent basis. In addition to reducing the leakage of sensitive data, such as patient medical records and other credentials, it is used to improve transparency and accountability, risk assessment by identifying data consumption, detection, prevention, and management of suspicious fraud, waste, and abuse. This market includes a variety of products and services intended to identify, stop, and reduce fraudulent activity in the healthcare sector. The healthcare industry's use of new technologies such as machine learning and artificial intelligence is expected to propel the market for healthcare fraud detection toward significant growth. The increased focus on analysis, service development, insurance claim reviews, and the necessity of upholding payment integrity all contribute to this growth direction.
Report Coverage
This research report categorizes the market for the global healthcare fraud detection market based on various segments and regions forecasts revenue growth and analyzes trends in each submarket. The report analyses the key growth drivers, opportunities, and challenges influencing the global healthcare fraud detection market. Recent market developments and competitive strategies such as expansion, product launch, and development, partnership, merger, and acquisition have been included to draw the competitive landscape in the market. The report strategically identifies and profiles the key market players and analyses their core competencies in each sub-segment of the global healthcare fraud detection market.
Global Healthcare Fraud Detection Market Report Coverage
| Report Coverage | Details |
|---|---|
| Base Year: | 2023 |
| Market Size in 2023: | USD 2.25 Billion |
| Forecast Period: | 2023 - 2033 |
| Forecast Period CAGR 2023 - 2033 : | 22.13% |
| 2033 Value Projection: | USD 16.61 Billion |
| Historical Data for: | 2019 - 2022 |
| No. of Pages: | 245 |
| Tables, Charts & Figures: | 110 |
| Segments covered: | By Type, By Delivery Model, By Application, By End User, By Region |
| Companies covered:: | IBM Corporation, Wipro Limited, HCL Technologies, Exlservice Holdings Inc., LexisNexis, Verscend Technologies, Mckesson, Conduent, Cotiviti Inc., OSP Labs, SAS Institute, Inc., International Business Machines Corporation, Scioinspire CORP, FAIR ISAAC Corporation, Others, and |
| Pitfalls & Challenges: | COVID-19 Empact, Challenges, Future, Growth, & Analysis |
Get more details on this report -
Driving Factors
The demand for healthcare fraud detection solutions is rising as a result of a rise in the number of patients looking for health insurance. This is one of the main reasons driving the market, along with the expanding prepayment review model in the healthcare sector. Furthermore, the global increase in frauds involving pharmacy claims is driving the market's expansion. Because more individuals are using health insurance, there is more pressure to prevent abuse and fraud, and there is an increase in healthcare fraud, the global market for healthcare fraud detection is growing.
Restraining Factors
The complexity and diversity of healthcare fraud schemes pose a considerable issue, as they frequently change in response to detection techniques and make it challenging for fraud detection technologies to stay up to date. Furthermore, the sheer volume and unpredictability of healthcare data provide difficulties for data integration, quality, and interoperability, which reduce the efficiency of analytics and algorithms for detecting fraud.
Market Segmentation
The global healthcare fraud detection market share is classified into type, delivery model, application, and end user.
- The descriptive analytics segment is dominates the market with the largest market share through the forecast period.
Based on the type, the global healthcare fraud detection market is categorized into descriptive analytics, predictive analytics, and prescriptive analytics. Among these, the descriptive analytics segment dominates the market with the largest market share through the forecast period. This is due to the solutions for descriptive analytics ease of use and their uncomplicated integration with other information sources to generate expressive insights. An increasing amount of clinical decisions and their effects on overall patient outcomes, care quality, and service performance are being evaluated through the use of descriptive analytics.
- The on-premises segment is predicted to dominate the highest revenue share through the forecast period.
Based on the delivery model, the global healthcare fraud detection market is categorized into on-premises, cloud-based, and others. Among these, the on-premises segment is predicted to dominate the highest revenue share through the forecast period. Hospitals and other institutions may easily access the data on the site, which has improved record-keeping and data monitoring, among other reasons. This model is preferred by organizations that prefer to keep direct control over their data security and compliance procedures, especially those that handle sensitive patient data or operate in areas with strict regulations, prefer this approach.
- The insurance claims review segment is accounted for the largest revenue share through the forecast period.
Based on the applications, the global healthcare fraud detection market is categorized into insurance claims review, pharmacy billing issues, payment integrity, and others. Among these, the insurance claims review segment is accounted for the largest revenue share through the forecast period. More people are purchasing health insurance, which in turn leads to an increase in the number of false claims. Prepayment review and post-payment review comprise the remaining portion of the section. Because of the increasing demand from healthcare providers, the prepayment review category is probably going to increase at the fastest rate of return.
- The public and government agencies segment is anticipated to grow at the fastest CAGR growth through the forecast period.
Based on the end user, the global healthcare fraud detection market is categorized into private insurance payers, public and government agencies, third party service providers, and others. Among these, the public and government agencies segment is anticipated to grow at the fastest CAGR growth through the forecast period. The main causes of the high percentage are the greater number of patients in government hospitals and the increased susceptibility of government institutions to fraud because of a lack of highly developed technology infrastructure, particularly in developing countries.
Regional Segment Analysis of the Global Healthcare Fraud Detection Market
- North America (U.S., Canada, Mexico)
- Europe (Germany, France, U.K., Italy, Spain, Rest of Europe)
- Asia-Pacific (China, Japan, India, Rest of APAC)
- South America (Brazil and the Rest of South America)
- The Middle East and Africa (UAE, South Africa, Rest of MEA)
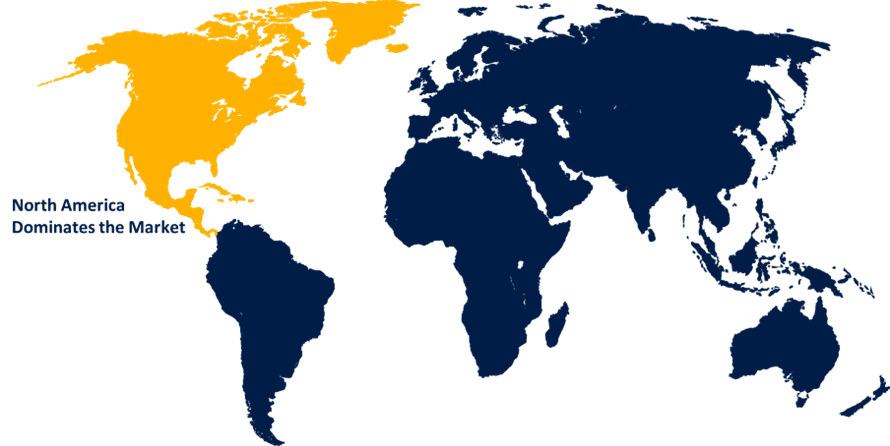
North America is anticipated to hold the largest share of the global healthcare fraud detection market over the predicted timeframe.
Get more details on this report -
North America is anticipated to hold the largest share of the global healthcare fraud detection market over the predicted timeframe. The strict regulatory frameworks and the increasing number of advanced healthcare systems define the fraud detection market. The region has experienced a notable uptake of fraud detection technologies due to legislative regulations including the Affordable Care Act and the False Claims Act. Additionally, the adoption of advanced fraud detection technologies utilizing artificial intelligence and data analytics has been made easier by an established healthcare infrastructure and a high degree of digitalization in healthcare procedures.
Europe is expected to grow at the fastest CAGR growth of the global healthcare fraud detection market during the forecast period. In similar ways, insurance coverage for patient maintenance during hospitalization is becoming more widely adopted due to the rising prevalence of chronic illnesses. For example, almost 50 million people in Europe are afflicted with various chronic illnesses. The demand for health coverage is driven by the annual increase in surgical procedures performed in European countries, which supports regional market growth.
Competitive Analysis:
The report offers the appropriate analysis of the key organizations/companies involved within the global healthcare fraud detection market along with a comparative evaluation primarily based on their product offering, business overviews, geographic presence, enterprise strategies, segment market share, and SWOT analysis. The report also provides an elaborative analysis focusing on the current news and developments of the companies, which includes product development, innovations, joint ventures, partnerships, mergers & acquisitions, strategic alliances, and others. This allows for the evaluation of the overall competition within the market.
List of Key Companies
- IBM Corporation
- Wipro Limited
- HCL Technologies
- Exlservice Holdings Inc.
- LexisNexis
- Verscend Technologies
- Mckesson
- Conduent
- Cotiviti Inc.
- OSP Labs
- SAS Institute, Inc.
- International Business Machines Corporation
- Scioinspire CORP
- FAIR ISAAC Corporation
- Others
Key Target Audience
- Market Players
- Investors
- End-users
- Government Authorities
- Consulting And Research Firm
- Venture capitalists
- Value-Added Resellers (VARs)
Recent Developments
- In June 2023, Payrailz Fraud Monitor, a cloud-native, AI-powered part of the Payrailz Digital Payments Platform, was presented by Jack Henry. This function starts detecting fraudulent activity in real-time as soon as a payment transaction is initiated.
- In February 2022, an across-the-industry effort was launched by the Canadian Life and Health Insurance Association (CLHIA) to combine claims data and make use of cutting-edge AI technologies to improve benefits fraud identification and investigation.
Market Segment
This study forecasts revenue at global, regional, and country levels from 2020 to 2033. Spherical Insights has segmented the global healthcare fraud detection market based on the below-mentioned segments:
Global Healthcare Fraud Detection Market, By Type
- Descriptive Analytics
- Predictive Analytics
- Prescriptive Analytics
Global Healthcare Fraud Detection Market, By Delivery Model
- On-Premises
- Cloud-Based
- Others
Global Healthcare Fraud Detection Market, By Application
- Insurance Claims Review
- Pharmacy Billing Issues
- Payment Integrity
- Others
Global Healthcare Fraud Detection Market, By End User
- Private Insurance Payers
- Public And Government Agencies
- Third Party Service Providers
- Others
Global Healthcare Fraud Detection Market, By Regional
- North America
- US
- Canada
- Mexico
- Europe
- Germany
- UK
- France
- Italy
- Spain
- Russia
- Rest of Europe
- Asia Pacific
- China
- Japan
- India
- South Korea
- Australia
- Rest of Asia Pacific
- South America
- Brazil
- Argentina
- Rest of South America
- Middle East & Africa
- UAE
- Saudi Arabia
- Qatar
- South Africa
- Rest of the Middle East & Africa
Frequently Asked Questions (FAQ)
-
1.What is the CAGR of the global healthcare fraud detection market?The global healthcare fraud detection market is projected to expand at a 22.13% during the forecast period.
-
2.Who are the top key players in the global healthcare fraud detection market?The key players in the global healthcare fraud detection market are IBM Corporation, Wipro Limited, HCL Technologies, Exlservice Holdings Inc., LexisNexis, Verscend Technologies, Mckesson, Conduent, Cotiviti Inc., OSP Labs, SAS Institute Inc., International Business Machines Corporation, Scioinspire CORP, FAIR ISAAC Corporation.
-
3.Which region is expected to hold the largest share in the global healthcare fraud detection market?The North America region is expected to hold the largest share of the global healthcare fraud detection market.
Need help to buy this report?